August 15, 2025

If you’re a commercial driver, you already know your physical and mental health are closely watched. But did you know that some prescription medications can affect your ability to keep your medical card?
Let’s talk about which medications get flagged under Federal Motor Carrier guidelines, what your responsibilities are, and why communication is key—for your safety and your career.
Certain medications are flagged for medical examiners to review more closely. These don’t automatically disqualify you from driving, but they do require additional evaluation.
Here are some examples:
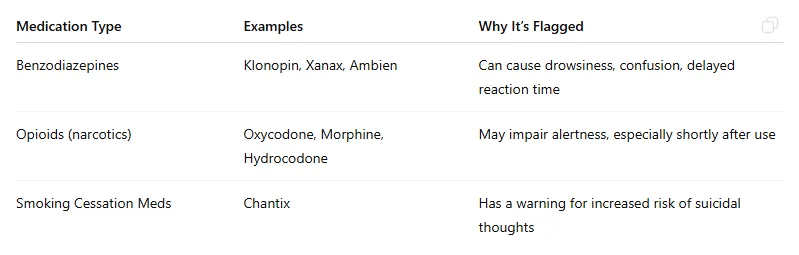
These meds don’t always mean you’ll lose your medical card, but they do signal: “Hey, this driver might need a closer look before we say it’s safe to drive.”
FMCSA has clear guidance when it comes to pain meds:
Even though these guidelines exist, most drivers and many employers don’t realize them. This is critical information—especially when medication labels say, “Do not operate machinery.”
Under FMCSA rules, drivers must report:
This includes letting your employer know if you’re using a sedating medication—even if it’s prescribed and legal. Some companies even put this in their work policies as a condition of employment.
But here’s the issue…
This is where things can get sticky.
Many supervisors don’t know what to do when a driver says, “Hey, just so you know—I’m taking medication that causes drowsiness.”
Should they send you home? Report it to a medical examiner? Call HR? That uncertainty is dangerous for both safety and compliance.
That’s why driver training programs should include how and when to report medications—and what supervisors are supposed to do with that info.
Some medications come with a black box warning, such as the potential for suicidal thoughts. One example is Chantix, a common medication to help people quit smoking.
Because of this kind of warning, Chantix and similar meds get flagged by:
All three require medical certifications, and any med that may impair mood, alertness, or stability will be scrutinized closely.
If you’re a driver or work in a safety-sensitive role, it’s not enough to just take your meds as prescribed. You also need to:
Your health and your job are both important. It’s possible to manage one without compromising the other, as long as you stay informed and get support where needed.


